Metatarsal fractures
Introduction
- Common injuries
- Occur in isolation or concomitant with other foot injuries
- 10x more common than Lisfranc injuries
- 5th metatarsal (MT) is most commonly injured
Mechanism of Injury
Acute fractures
- Direct trauma: falls, motor vehicle accidents, crush, impact of heavy objects etc
- Indirect trauma: falls on the plantar flexed and fixed foot or inversion injuries
Stress fractures
- Repetitive strain or trauma
5th MT fractures
- classically result from indirect inversion injuries
Cadaveric studies suggest that the lateral band of the plantar aponeurosis tethers the 5th MT base causing tuberosity avulsion fractures, with the peroneus brevis tendon acting as the major deforming force to further displacement.
Imaging
X-ray
- AP, lateral, and oblique radiographs of the foot
- ideally weight-bearing
CT
- helpful with comminuted or intra-articular fractures
- assessment of delayed / non-union
Classification
- 1st to 4th MT fractures by anatomical location
- 5th MT fractures by specific anatomical location:
- Tuberosity or avulsion fractures
- Junction of metaphysis / diaphysis
- Proximal diaphysis
- Shaft fractures
Lawrence and Botte divided the proximal fifth metatarsal into three distinct fracture zones
- Zone I - avulsion fracture of the tuberosity (more than 90% of fractures in their study)
- [These can be further divided into intra- or extra-articular]
- Zone II - the metadiaphyseal region at the level of 4th/5th intermetatarsal joint (“Jones” fracture)
- Zone III - the proximal diaphyseal region (often stress fractures)
Other 5th MT classifications
DeLee et al: separated proximal fifth metatarsal fractures further
Torg et al: helps determine fracture age and healing potential based on radiographic appearance:
- Type I: acute fractures without intramedullary sclerosis
- Type II: delayed fracture healing with a widened fracture line and intramedullary sclerosis
- Type III: non-unions with obliteration of the intramedullary canal by sclerosis
Treatment
- Most fractures heal uneventfully with conservative treatment
- However, a small percentage may lead to nonunion or malunion, causing pain and disability
Non-operative management
Indications
- Undisplaced / minimally displaced fractures
- Preserved sagittal plane alignment
Method
- Splintage for 4-6 weeks
- stiff-soled shoe, plaster shoe, walker boot
- below-knee lightweight cast
- Weight bearing as comfort allows (‘unrestricted’)
- Most fractures heal within 6 weeks with return to normal activities soon after
Outcomes
- Highly satisfactory
- Malunion may cause metatarsalgia or necessitate future surgery
Surgical management
Indications
- Open fractures
- Significantly displaced fractures
- Mal-rotation
- Fracture angulation >10 degrees
- sagittal plane displacement is poorly tolerated
- alters the weight-bearing relationship of the MT heads
- may result in painful callosities and metatarsalgia
- Transverse plane displacement is better tolerated
- can be associated with interdigital nerve impingement
- Multiple metatarsal fractures (minimal objective evidence)
- Non- or delayed union
Goals
- Restore length, alignment, rotation
- Balance the MT head arcade
- Promote bone healing
Surgical options
- Dependent upon:
- metatarsal(s) involved
- fracture pattern
- soft tissue envelope
- Closed reduction and temporising K-wire fixation
- restore length and alignment
- avoid fixing the toe in dorsiflexion
- Lag screw fixation for spiral / oblique fractures
- Plate +/- screw fixation
Case 1 - Pedestrian hit by car

Figure 1: Multiple metatarsal fractures

Figure 2: CT demonstrates significant malalignment

Figure 3: 3 months post fixation
Case 2 - delayed presentation of inversion injury

Figure 4: Discplaced, intra-articular, communted fracture with signs of early sclerosis

Figure 5: 3 months following compression screw fixation with signs of early failure / non-union
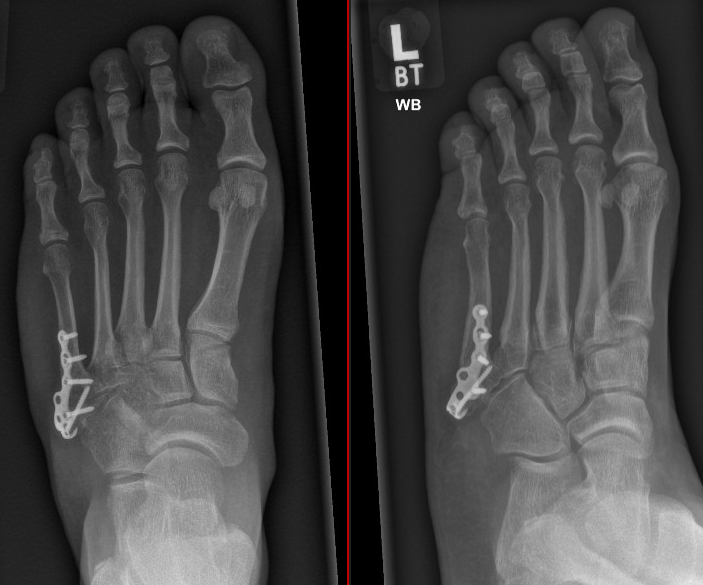
Figure 6: 3 months following revision fixation and cancellous autograft (from heel)
Jones fracture
- Requires special mention
- Fractures of 5th MT occurring in Zone II at the junction of the metaphysis and diaphysis
- First described by Sir Robert Jones (1902)
- Mechanism is usually by adduction and axial loading of a plantarflexed foot
- Location is a watershed area with relative hypovascularity → increased risk of non-union
- Therefore needs a more watchful approach
Treatment
Non-operative management
- Undisplaced or minimally displaced fractures
- Immobilisation period of 6 weeks
- non-weight bearing cast or weight bearing in a boot
- Extracorporeal shockwave therapy
- can be used for non-unions
- limited evidence suggests excellent union rates compared to surgical treatment; lower complication rates
Surgical management
- Displaced fractures
- Symptomatic non-union
- Patients requiring earlier return to activity e.g. high-level athletes, patients with other occupational needs
- Intra-medullary screw (solid or cannulated, partially-threaded)
- Plating
- + bone grafting for non-unions (e.g. local cancellous bone)
- Tension band wiring
- Evidence suggests, compared with non-operative management:
- faster return to sports
- higher union rates (96% versus 76%)
MCQ questions
The Jones fracture is a common fracture of the fifth metatarsal that is associated with high rates of non-union. Which zone of the Lawrence and Botte classification does this fracture affect?
True or false?
- All metatarsal fractures need to be immobilised in a non-weight bearing cast.
- Displacement in the sagittal plane of a metatarsal fracture is an indication for surgical management.
- The Torg classification classifies metatarsal fractures based on the location of the fracture.
- All base of fifth metatarsal fractures need surgical treatment.
- Surgical management of base of fifth metatarsal fractures is correlated with higher union rate and faster return to sports.
References
Pituckanotai et al. Comparative Outcomes of Cast and Removable Support in Fracture Fifth Metatarsal Bone: Systematic Review and Meta-Analysis. The Journal of Foot & Ankle Surgery 57 (2018) 982–986 https://doi.org/10.1053/j.jfas.2018.03.018
Roche AJ, Calder JD: Treatment and return to sport following a Jones fracture of the fifth metatarsal: a systematic review. Knee Surg Sports Traumatol Arthrosc 2013; 21: pp. 1307-1315. Epub 2012 Sep 6
Hunt KJ, Anderson RB: Treatment of Jones fracture nonunions and refractures in the elite athlete: outcomes of intramedullary screw fixation with bone grafting. Am J Sports Med 2011; 39: pp. 1948-1954. Epub 2011 Jun 1
Rammelt S, Heineck J, Zwipp H. Metatarsal fractures. Injury 2004; 35: pp. SB77-SB86
Smith T, Clark A, Hing C. Interventions for treating proximal fifth metatarsal fractures in adults: A meta-analysis of the current evidence-base. Foot Ankle Surg. 2011 Dec;17(4):300-7
Furia JP, Juliano PJ, Wade AM, et. al.: Shock wave therapy compared with intramedullary screw fixation for nonunion of proximal fifth metatarsal metaphyseal-diaphyseal fractures. J Bone Joint Surg Am 2010; 92: pp. 846-854
Mologne TS, Lundeen JM, Clapper MF, et. al.: Early screw fixation versus casting in the treatment of acute Jones fractures. Am J Sports Med 2005; 33: pp. 970-975. Epub 2005 May 11
Theodorou DJ, Theodorou SJ, Kakitsubata Y, et. al.: Fractures of proximal portion of fifth metatarsal bone: anatomic and imaging evidence of a pathogenesis of avulsion of the plantar aponeurosis and the short peroneal muscle tendon. Radiology 2003; 226: pp. 857-865
Lawrence SJ, Botte MJ: Jones’ fractures and related fractures of the proximal fifth metatarsal. Foot Ankle 1993; 14: pp. 358-365
Smith JW, Arnoczky SP, Hersh A: The intraosseous blood supply of the fifth metatarsal: implications for proximal fracture healing. Foot Ankle 1992; 13: pp. 143-152
Torg JS, Balduini FC, Zelko RR, et. al.: Fractures of the base of the fifth metatarsal distal to the tuberosity. Classification and guidelines for non-surgical and surgical management. J Bone Joint Surg Am 1984; 66: pp. 209-214
Jones R: Fracture of the base of the fifth metatarsal bone by indirect violence. Ann Surg 1902; 35: pp. 697-700