Part 3: Anatomical Variation and Bone Density
ANATOMICAL VARIATION
Accessory ossicles
- Unfused secondary ossification centres; common in the foot
- Usually asymptomatic but a small proportion may be symptomatic, particularly following (minor) trauma or sporting activity; needs to be differentiated from a fracture
Accessory ossicle:
Well defined sclerotic margin with normal adjacent bones
Recent fracture:
Tender, with at least one edge where the sclerotic margin is absent and irregular margin of an adjacent bone indicating the origin of the fracture fragment

Common accessory ossicles:
- os trigonum
- os supratalare
- os supranaviculare
- os calcaneus secundaris
- os peroneum
- os vesalianum
- os naviculare
Os trigonum
Located posterior to the talus; ~8% of the population.
May cause posterior ankle pain if compressed between the posterior tibia and posterior calcaneus during forced plantar flexion, as occurs in footballers and ballet dancers; referred to as os trigonum syndrome or posterior ankle impingement.
Os peroneum
Located in the peroneal groove of the cuboid, embedded in the peroneus longus tendon. Associated with peroneus longus tenosynovitis and tear.
Os vesalianum
Located at the fifth metatarsal base. Must be differentiated from an avulsion fracture;
a fracture has a longitudinal orientation and an irregular outline, compared to the transverse orientation and smooth contour of the ossicle.
Os naviculare
Located proximal to the navicular tuberosity (medial side); often embedded in distal tibialis posterior tendon.
Synchondrosis can be ‘tweaked’ by minor trauma, leading to painful micro-movement and subsequent degenerative changes between the accessory ossicle and navicular; development of bursitis and localised swelling / prominence. May be associated with a higher incidence of tibialis posterior tendinopathy and tears.
Hallux Sesamoids
Symptomatic sesamoids may be due to fractures, osteonecrosis, inflammation (sesamoiditis), infection and involvement in degenerative or inflammatory joint disease.
Sesamoiditis
Sclerotic, irregular, fragmented (MRI more sensitive in early phase)
Sesamoid fracture
Commonly mistaken for a bipartite sesamoid.
Bipartite sesamoid:
Smooth, well-corticated transverse lucency with rounded margins; bipartite usually larger than single sesamoid thus the sum of the two parts is greater than the adjacent sesamoid.
Sesamoid fracture:
Painful, non-corticated fracture line separating irregular opposing sesamoid fragments with sharp edges.

Bipartite sesamoid Sesamoid fracture
Tarsal Coalitions
- Occur in about 6% of the population
- Thought to represent failure of proper segmentation of the tarsal bones
- May be fibrous (syndesmosis), cartilaginous (synchondrosis) or osseous (synostosis)
- May be bilateral and result in restricted subtalar joint motion
Calcaneo-navicular coalition
- Best seen on oblique views
- ‘Anterior nose’ sign or ‘anteater’ sign = anterior extension of enlarged anterolateral calcaneal process
- Osseous coalition: connecting osseous bar (bony bridge) between anterior calcaneal process and navicular
- Fibrous coalition: Sclerosis and irregularity at coalition interface (non-osseous coalition)
- Possible hypoplastic talar head
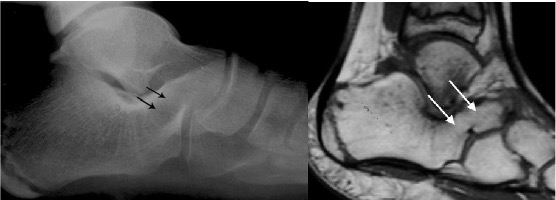
Osseous calcaneo-navicular coalition (arrows)
Talo-calcaneal coalition
- Occurs on the medial side of the talus
- Usually at the middle subtalar facet
- Prominent talar beak arising from dorsal talar head or neck (not obvious in this image)
- C sign – Formed by prominence of inferior border of sustentaculum and talar dome on lateral projection (NB this is not diagnostic of coalition as it can often be seen with a valgus heel e.g. flat foot)

Talocalcaneal coalition with characteristic C shape (arrows) on lateral view
Ankle impingement
Usually due to repeated micro trauma or chronic traumatic injuries where soft tissue is repeatedly trapped between the tibia and talus.
Anterior impingement
- Osseous spurs arising from anterior distal tibia and dorsal talar neck
- Corresponding ‘Divot’ sign may be seen in talar neck
- “Footballer’s ankle” is anterior impingement caused by repetitive micro-trauma

Anterior impingement with anterior distal tibial osseous spur (arrow)
Posterior impingement
Can be caused by:
- prominent os trigonum
- Stieda process (elongation of the lateral tubercle of the posterior talar process)
- posterior talar fracture
- ossification
- soft tissue impingement between the posterior tibia and talus on plantar flexion

Posterior impingement with prominent os trigonum (arrow)
Haglund Deformity
- Prominent bony protrusion of posterior superior calcaneal tuberosity
- Soft tissue swelling of distal Achilles tendinopathy and retrocalcaneal bursitis resulting in Haglund’s syndrome
- Problems with footwear

Haglund’s deformity (thin arrow) with soft tissue swelling (bold arrowheads)
BONE DENSITY
Osteopenia: reduced bone density; may be a pre-cursor to:
Osteoporosis: diminished quantity and density of normal bone
Osteomalacia: may have normal or reduced density but weak due to defective bone mineralisation
Regional osteopenia confined to the foot may be seen with:
Disuse osteoporosis: usually appears after 8 weeks of immobilization, typically with fractures
Reflex sympathetic dystrophy (Sudeck’s atrophy): mediated via a neurovascular mechanism usually following trauma with pain and soft tissue swelling often out of proportion to injury
Regional migratory osteoporosis: unknown aetiology typically occurring in middle aged males characterized by pain and localised osteoporosis which migrates from one joint to another
Osteosclerosis
- Increased bone density
- Focal sclerotic areas in the foot may be seen with:
- chronic sclerosing osteomyelitis
- Charcot foot
- chronic avascular necrosis
- healing stress fractures
- sclerotic metastases
- renal osteodystrophy